“`html
How to Properly Calculate Cardiac Output: 5 Effective Methods for Improved Heart Health in 2025
Understanding how to calculate cardiac output is critical for assessing heart health and function. Cardiac output is a vital sign that measures the average volume of blood the heart pumps in a minute, reflecting the heart’s overall efficiency. Whether you are a medical professional, a fitness enthusiast, or simply someone looking to improve your health, knowing the cardiac output calculation methods will empower you to better monitor and understand cardiac physiology.
1. The Basics of Cardiac Output
Before diving into the specifics of measurement, it’s essential to grasp the fundamentals. The cardiac output formula is straightforward: CO = SV x HR. Here, CO represents cardiac output, SV stands for stroke volume (the amount of blood pumped by the heart with each beat), and HR is the heart rate (beats per minute). Understanding this formula is the foundation for further assessment techniques.
Stroke Volume Importance
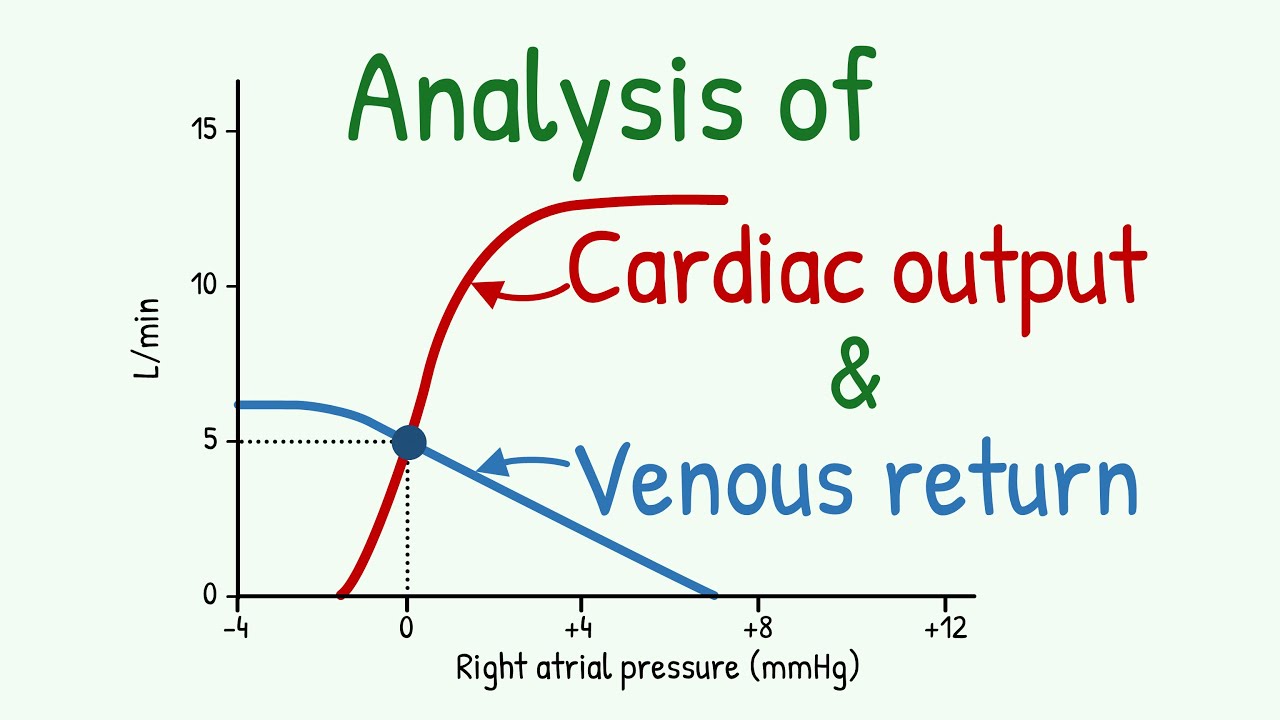
Stroke volume is crucial when calculating cardiac output, as it indicates the volume of blood ejected by the heart’s ventricles. Factors affecting stroke volume include venous return, myocardial contractility, and systemic vascular resistance. For example, in athletes, improved stroke volume results from enhanced left ventricular function, directly influencing cardiac performance. Regular monitoring can unveil a lot about your heart’s efficiency.
Significance of Heart Rate
The heart rate, another component of the cardiac output equation, directly impacts how much blood is pumped per minute. Conditions like arrhythmias or stress can dramatically alter heart rate and, thus, cardiac output. Monitoring heart rate variability gives insights into your cardiovascular stability. High heart rates can lead to low stroke volume if the heart doesn’t have adequate time to fill between beats, complicating blood circulation.
Clinical Implications
Understanding the relation between cardiac output and blood pressure is vital in a clinical setting. Low cardiac output can indicate poor heart function, leading to inadequate oxygen delivery to tissues, which can affect overall health significantly. Constant assessment helps to preemptively identify possible complications and initiate necessary interventions.
2. Methods of Measuring Cardiac Output
Various techniques to measure cardiac output exist, each with its strengths and applications. This section will review both invasive and non-invasive measurement techniques, focusing on their relevance to clinical assessments.
Echocardiography
Echocardiography is a widely used non-invasive method that employs ultrasound waves to produce moving images of the heart. It assesses dimensions, structural changes, and functional capacities of cardiac performance. Using Doppler ultrasound, echocardiography can estimate blood flow and, consequently, cardiac output by evaluating stroke volume and heart rate without direct access to the chamber.
Invasive Monitoring Techniques
For more accurate measurements, especially in critically ill patients, invasive monitoring techniques such as cardiac catheterization using the thermodilution method may be used. This procedure involves inserting a catheter into a blood vessel and measuring the warmth of injected saline over time to calculate stroke volume and derive cardiac output.
Non-invasive Techniques: Bioimpedance and Others
Non-invasive techniques like bioimpedance provide alternative methods to assess cardiac output without the risks associated with invasive procedures. Bioimpedance measures the resistance of body tissues to an electrical current, which can then estimate blood volume and flow. Being less intrusive, these methods allow for continuous monitoring in varied environments like home or outpatient settings.
3. Factors Affecting Cardiac Output
Multiple external and internal factors can influence cardiac output, revolving around heart function, blood volume, and overall cardiovascular health. Recognition of these factors is essential for accurate assessment and management.
Impact of Exercise on Cardiac Output
Exercise induces physiological changes that enhance cardiac output. It increases heart rate and stroke volume due to improved myocardial efficiency and blood volume during intense activities, thereby maximizing oxygen delivery to tissues. Individuals engaged in regular cardiovascular fitness training can often observe significantly higher values for stroke volume and heart rate, indicating robust cardiac performance.
Cardiac Function in Disease States
In individuals with chronic conditions, such as heart disease, monitoring cardiac output in heart disease is paramount because reduced efficiency can lead to severe complications. Low cardiac output may result from a weak myocardium or compromised coronary artery flow. Understanding the heart’s current workload and its limitations aids in the development of specific interventions.
Understanding Hemodynamic Parameters
Other hemodynamic parameters also interact with cardiac output, including systemic vascular resistance and pulmonary circulation dynamics. Variability in blood flow can alter overall cardiac stability, making it crucial for healthcare professionals to comprehensively analyze these dynamics when assessing physiological measurements during a cardiovascular assessment.
4. Advanced Techniques in Cardiac Output Assessment
The evolution of cardiac output measurement is advancing rapidly, integrating both technology and methodology for superior patient outcomes. These techniques are especially valuable in high-stakes environments like critical care.
Pulse Contour Analysis
Pulse contour analysis relies on artery pressure waveforms to provide continuous cardiac output monitoring. This method allows for real-time physiological data and interpretation, granting healthcare providers immediate insight into cardiac performance evaluation. Its ability to track changes helps detect worsening patient conditions swiftly, resulting in timely interventions.
Emerging Trends in Cardiac Care
Technology innovations continue to refine traditional methods. Continuous wave Doppler and advanced bioengineering techniques have opened avenues for personalized assessment strategies addressing individual physiological needs. Such innovations contribute to better outcomes during health interventions and surgical procedures, emphasizing the increasing importance of cardiac assessment tools.
Clinical Guidelines for Cardiac Output Measurement
Following clinical guidelines for cardiac output measurement is essential for ensuring accuracy and reliability in results across various health settings. Guidelines offer protocols on patient preparation, technique application, and result interpretation, all of which contribute significantly to patient-centered cardiac assessments.
Key Takeaways
- Understanding cardiac output and its calculation methods is essential for cardiovascular assessment.
- Techniques like echocardiography and invasive monitoring can provide various insights into cardiac function.
- Many factors influence cardiac output, making it crucial to evaluate these during clinical assessments.
- Emerging technologies are vital in enhancing the accuracy and safety of cardiac monitoring.
- Following established clinical guidelines ensures consistent and interpretable cardiac output results.
FAQ
1. What is the importance of cardiac output in assessing heart health?
Cardiac output is fundamental in evaluating how effectively the heart delivers oxygenated blood throughout the body. Monitoring cardiac output helps identify heart-related conditions and informs treatment decisions.
2. What methods can I use to calculate my cardiac output at home?
While direct measurement of cardiac output at home is challenging, using heart rate and understanding your estimated stroke volume can provide insights. Wearable fitness devices that track heart rate variability can assist in this self-assessment.
3. How does exercise affect cardiac output?
Exercise typically increases both heart rate and stroke volume, leading to higher cardiac output. Engaging in regular physical activity strengthens the heart muscle, improving myocardial function over time.
4. What are the complications of low cardiac output?
Low cardiac output may result in inadequate oxygen delivery, leading to symptoms like fatigue, confusion, and shortness of breath. Severe cases can cause organ damage and require immediate medical intervention.
5. Can echocardiographic assessment be performed in outpatient settings?
Yes, echocardiography can be performed in outpatient settings, allowing for detailed assessments and ongoing monitoring of cardiac health without the need for hospitalization.
“`